
Autoimmune polyendocrine syndrome
| Autoimmune polyendocrine syndrome | |
|---|---|
| Other names | Autoimmune polyglandular syndromes (APSs) |
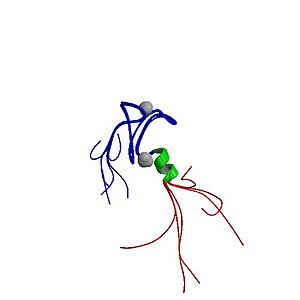 | |
| The autoimmune regulator protein (from the AIRE gene, which causes autoimmune polyendocrine syndrome type 1 when non-functional) | |
| Specialty |
Endocrinology |
| Types |
APS type1, APS type 2, IPEX syndrome |
| Causes | FOXP3 gene is involved in the mechanism |
| Diagnostic method | Endoscopic, CT scan |
| Treatment | Depends on type |
Autoimmune polyendocrine syndromes (APSs), also called polyglandular autoimmune syndromes (PGASs) or polyendocrine autoimmune syndromes (PASs), are a heterogeneous group of rare diseases characterized by autoimmune activity against more than one endocrine organ, although non-endocrine organs can be affected. There are three types of APS, and there are a number of other diseases which involve endocrine autoimmunity.
Types
- Autoimmune polyendocrine syndrome type 1, an autosomal recessive syndrome due to mutation of the AIRE gene resulting in hypoparathyroidism, adrenal insufficiency, hypogonadism, vitiligo, candidiasis and others.
- Autoimmune polyendocrine syndrome type 2, an autosomal dominant syndrome due to multifactorial gene involvement resulting in adrenal insufficiency plus hypothyroidism and/or type 1 diabetes.
- Immunodysregulation polyendocrinopathy enteropathy X-linked syndrome (IPEX syndrome) is X-linked recessive due to mutation of the FOXP3 gene on the X chromosome. Most patients develop diabetes and diarrhea and many die due to autoimmune activity against many organs. Boys are affected, while girls are carriers and might experience mild disease.
Cause
Each "type" of this condition has a different genetic cause. IPEX syndrome is inherited in males by an X-linked recessive process. The FOXP3 gene, whose cytogenetic location is Xp11.23, is involved in the mechanism of the IPEX condition.
Diagnosis
Diagnosis for type 1 of this condition for example, sees that the following methods/tests are available:
- Endoscopic
- CT scan
- Histologic test
Differential diagnosis
For this condition, differential diagnosis sees that the following should be considered:
- CD25 deficiency
- STAT5B deficiency
- Severe combined immunodeficiency
- X linked thrombocytopenia
Management
Immunosuppressive therapy may be used in type I of this condition.Ketoconazole can also be used for type I under certain conditions.
The component diseases are managed as usual; the challenge is to detect the possibility of any of the syndromes and to anticipate other manifestations. For example, in a person with known type 2 autoimmune polyendocrine syndrome but no features of Addison's disease, regular screening for antibodies against 21-hydroxylase may prompt early intervention and hydrocortisone replacement to prevent characteristic crises
See also
Further reading
- Improda, Nicola; Capalbo, Donatella; Cirillo, Emilia; Cerbone, Manuela; Esposito, Andrea; Pignata, Claudio; Salerno, Mariacarolina (1 November 2014). "Cutaneous vasculitis in patients with autoimmune polyendocrine syndrome type 1: report of a case and brief review of the literature". BMC Pediatrics. 14: 272. doi:10.1186/1471-2431-14-272. ISSN 1471-2431. PMC 4286916. PMID 25361846.
- Shoenfeld, Yehuda; Cervera, Ricard; Gershwin, M. Eric (2008). Diagnostic Criteria in Autoimmune Diseases. Springer Science & Business Media. ISBN 9781603272858.
External links
- Diseases Database (DDB): 29690
- PubMed
| Classification | |
|---|---|
| External resources |
|
Disorders involving multiple endocrine glands
| |
|---|---|
|
Type I/allergy/atopy (IgE) |
|
||||||||
|---|---|---|---|---|---|---|---|---|---|
|
Type II/ADCC |
|
||||||||
|
Type III (Immune complex) |
|
||||||||
|
Type IV/cell-mediated (T cells) |
|
||||||||
| Unknown/ multiple |
|
||||||||

