Orofacial pain
| Orofacial pain | |
|---|---|
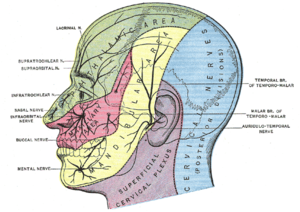 | |
| Dermatomes of the face. | |
| Specialty | ENT surgery, dentistry |
Orofacial pain is a general term covering any pain which is felt in the mouth, jaws and the face. Orofacial pain is a common symptom, and there are many causes.
Orofacial Pain (OFP) is the specialty of dentistry that encompasses the diagnosis, management and treatment of pain disorders of the jaw, mouth, face and associated regions. These disorders as they relate to orofacial pain include but are not limited to temporomandibular muscle and joint (TMJ) disorders, jaw movement disorders, neuropathic and neurovascular pain disorders, headache, and sleep disorders.
Classification
International Classification of Diseases (ICD-11) is a new classification coming into effect as of January 1, 2022. It includes chronic secondary headaches and orofacial pain. The classification has been established by a close cooperation between International Association for the Study of Pain (IASP), World Health Organization (WHO) and the International Headache Society (IHS).
There are 4 main classifications prior to ICD-11 which attempt to classify the causes of orofacial pain.
- The International Classification of Headache Disorders third edition (ICHD-3), a publication by the International Headache Society. https://ichd-3.org/
- The Classification of Chronic Pain Second Edition (Revised), a publication by the International Association for the Study of Pain.
- Orofacial Pain: Guidelines for Assessment, Diagnosis, and Management, Fifth Edition by American Academy of Orofacial Pain (AAOP): www.aaop.org.
- The Research Diagnostic Criteria for Temporomandibular Disorders (see TMD).
It has also been suggested that the most basic etiologic classification of orofacial pain is into the following 3 groups:
- Primarily somatic, arising from musculoskeletal (e.g. TMD pain or periodontal pain) or visceral structures (e.g. pulpal pain or pain from the salivary glands), and transmitted via an intact pain transmission and modulation system.
- Primarily neuropathic, which occurs as a result of abnormal or damaged pain pathways, e.g. a surgical or traumatic injury to a peripheral nerve.
- Primarily psychological, which is rare (See: psychogenic pain)
Diagnosis
Diagnosis of orofacial pain can be difficult and can require multiple examinations and histories provided by the patient. The pain history is essential and will indicate any further examinations required.
The correct diagnosis of orofacial pain requires an in-depth pain history which will include:
- Location of the pain
- Timing
- Duration
- Associated symptoms
- Exacerbating and alleviating factors
- Description of the type of pain experienced e.g. dull, aching, throbbing, burning, tingling or pulsating.
Other information and examinations include:
- Full medical history
- Full dental history
- Full social history
- Clinical examination
- Radiographic examination
Differential diagnosis
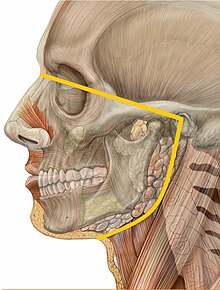
Clinical presentation of orofacial pain.
Dental related
- Pulpal
- Dentinal hypersensitivity resulting from
- Pulp disease (reversible and irreversible pulpitis) resulting from
- Caries
- Trauma
- Periapical pathology and periapical acute abscess
- Periodontal
- Periodontal abscess
- Pericoronitis and pericoronal abscess
- Cracked tooth syndrome
Non-dental related
- Musculoskeletal including Temporomandibular diseases (TMD)
- Neuralgias and neuropathies
- Trigeminal neuralgia
- Glossopharyngeal neuralgia
- Sphenopalatine Ganglion neuralgia
- Sluder's Neuralgia
- Mental nerve neuralgia
- Post-injury
- Burning mouth syndrome
- Postherpetic neuralgia
- Persistent idiopathic facial pain (atypical facial pain)
- Mucosal
- Traumatic, immunologic, infective, erosive, ulcerative and vesiculobullous lesions e.g. oral ulceration (e.g. aphthous stomatitis, erosive oral lichen planus, etc.)
- Psychosomatic
- Sinonasal
- Headaches
- Salivary gland disease
- Cardiac toothache
- Eagle syndrome
Management
A multi-disciplinary approach is needed for orofacial pain disorders involving both non-pharmacological and pharmacological approaches which can be applied to the specific type of disorder. Non-pharmacological approaches can include physical therapies and psychological support to effectively manage the facial pain and reduce the negative impact on quality of life and daily functioning. Self-management interventions, such as education, jaw posture relaxation, and cognitive or behavioral self regulation, have been shown to improve long-term outcomes for patients with orofacial pain, specifically in patients with TMD. Self-Administration of Sphenopalatine Ganglion Blocks (SPG or Pterygopalatine Ganglion) is an excellent approach to a wide variety of orofacial pain conditions.
Often chronic orofacial pain (lasting over 12 weeks) requires referral to a specialised branch of medicine or dentistry or continuation of treatment in a primary care setting, if symptoms cannot be managed otherwise.
- Oral and maxillofacial referral for TMD
- Primary care referral for tension-type headaches
- Neurology referral for migraines and cluster headaches
- Ear Nose and Throat referral for rhinosinusitis and midfacial segment pain
Epidemiology
Orofacial pain is common problem. For example, in the United States, one report estimated that 22% of the general population had experienced some form of facial pain at some point in the 6-month period before questioning, of which 12% was toothache. In the United Kingdom, 7% of the general population reported having some degree of chronic orofacial pain. Other reports indicate a prevalence of 10–15% for TMD in the general population.
A systematic review looking at the prevalence of orofacial pain found that highest prevalence was for pain on opening the mouth (21%-49%), muscle tenderness (17%-97%) and self-reported joint pain (5%-31%).
See also
External links
- BMJ Infographic - Identification and initial management of chronic orofacial pain
- Treating Sleep Apnea with Orofacial Myofunctional Therapy