
Thought disorder
| Thought disorder | |
|---|---|
| Other names | Formal thought disorder (FTD), thinking disorder |
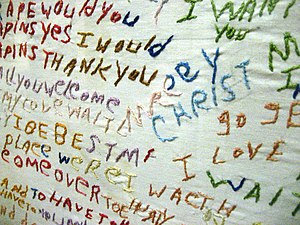 | |
| Cloth embroidered by a person diagnosed with schizophrenia; non-linear text has multiple colors of thread | |
| Specialty | Psychiatry, clinical psychology |
A thought disorder (TD) is a disturbance in cognition which affects language, thought and communication. Psychiatric and psychological glossaries in 2015 and 2017 identified thought disorders as encompassing poverty of ideas, neologisms, paralogia, word salad, and delusions - all disturbances of thought content and form. Two specific terms have been suggested - content thought disorder (CTD) and formal thought disorder (FTD). CTD has been defined as a thought disturbance characterized by multiple fragmented delusions, and the term thought disorder is often used to refer to an FTD: a disruption of the form (or structure) of thought. Also known as disorganized thinking, FTD results in disorganized speech and is recognized as a major feature of schizophrenia and other psychoses (including mood disorders, dementia, mania, and neurological diseases). Disorganized speech leads to an inference of disorganized thought. Thought disorders include derailment,pressured speech, poverty of speech, tangentiality, verbigeration, and thought blocking. One of the first known cases of thought disorders, or specifically OCD as we know it today, was in 1691. John Moore, who was a bishop, had a speech in front of Queen Mary II, about "religious melancholy."
Formal thought disorder affects the form (rather than of the content) of thought. Unlike hallucinations and delusions, it is an observable, objective sign of psychosis. FTD is a common core symptom of a psychotic disorder, and may be seen as a marker of severity and as an indicator of prognosis. It reflects a cluster of cognitive, linguistic, and affective disturbances that have generated research interest in the fields of cognitive neuroscience, neurolinguistics, and psychiatry.
Eugen Bleuler, who named schizophrenia, said that TD was its defining characteristic. Disturbances of thinking and speech, such as clanging or echolalia, may also be present in Tourette syndrome; other symptoms may be found in delirium. A clinical difference exists between these two groups. Patients with psychoses are less likely to show awareness or concern about disordered thinking, and those with other disorders are aware and concerned about not being able to think clearly.
Content thought disorder
Content thought disorder is a thought disturbance in which a person experiences multiple, fragmented delusions, typically a feature of schizophrenia and some other mental disorders which include obsessive-compulsive disorder and mania. At the core of thought content disorder are abnormal beliefs and convictions (after taking the person's culture and background into consideration) ranging from overvalued ideas to fixed delusions. These beliefs and delusions are typically non-specific diagnostically, even if some delusions are more prevalent in one disorder than another.
Neurotypical thought—consisting of awareness, concerns, beliefs, preoccupations, wishes, fantasies, imagination, and concepts—can be illogical, and can contain contradictory beliefs and prejudices or biases. Individuals vary considerably, and a person's thinking may also shift from time to time.
Content thought disorder is not limited to delusions. Other possible abnormalities include suicidal, violent, and homicidal ideas and:
- Preoccupation: centering thought on a particular idea in association with a strong affection
- Obsession: a persistent thought, idea, or image which is intrusive or inappropriate, and distressing or upsetting
- Compulsive behavior: the need to perform an act persistently and repetitively (without it necessarily leading to a reward or pleasure) to reduce distress
- Magical thinking: belief that one's thoughts alone can bring about effects in the world, or that thinking something corresponds with doing that thing
- Overvalued ideas: false or exaggerated belief held with conviction, but without delusional intensity
- Phobias: irrational fears of objects or circumstances
In psychosis, delusions are the most common thought content disorder. A delusion is a firm, fixed belief based on inadequate grounds, not amenable to rational argument or evidence to the contrary, which is out of sync with a person's regional, cultural, or educational background. Delusions are common in people with mania, depression, schizoaffective disorder, delirium, dementia, substance use disorders, schizophrenia, and delusional disorders. Common examples in a mental status examination include the following:
- Erotomania: belief that someone is in love with oneself
- Grandiose delusions: belief that one is the greatest, strongest, fastest, richest, or the most intelligent person ever
- Persecutory delusion: belief that the person, or someone to whom the person is close, is being malevolently treated in some way
- Ideas and delusions of reference: belief that insignificant remarks, coincidental events, or innocuous objects in one's environment have personal meaning or significance
- Thought broadcasting: belief that others can hear (or are aware of) one's thoughts
- Thought insertion: belief that one's thoughts are not one's own, but belong to someone else and have been inserted into one's mind
- Thought withdrawal: belief that thoughts have been "taken out" of one's mind, and one has no power over this
- Influence: belief that other people (or external agents) are covertly exerting power over oneself
- Outside control: belief that outside forces are controlling one's thoughts, feelings, and actions
- Infidelity: belief that a partner is cheating on oneself
- Somatic: belief that one has a disease or medical condition
- Nihilistic: belief that the mind, the body, the world at large, or parts thereof no longer exist
Formal thought disorder
Formal thought disorder (FTD) is also known as disorganized speech. Evidence of disorganized thinking, it is a hallmark feature of schizophrenia. FTD, a disorder of the form (rather than content) of thought, encompasses hallucinations and delusions and is an observable sign of psychosis. A common, core symptom of psychosis, it may be seen as a marker of severity and a predictor of prognosis. FTD reflects a cluster of cognitive, linguistic, and affective disturbances which has generated research interest from the fields of cognitive neuroscience, neurolinguistics, and psychiatry.
It can be subdivided into clusters of positive and negative symptoms and objective (rather than subjective) symptoms. On the scale of positive and negative symptoms, they have been grouped into positive formal thought disorder (posFTD) and negative formal thought disorder (negFTD). Positive subtypes were pressure of speech, tangentiality, derailment, incoherence, and illogicality; negative subtypes were poverty of speech and poverty of content. The two groups were posited to be at either end of a spectrum of normal speech, but later studies showed them to be poorly correlated. A comprehensive measure of FTD is the Thought and Language Disorder (TALD) Scale. The Kiddie Formal Thought Disorder Rating Scale (K-FTDS) can be used to assess the presence of formal thought disorder in children and their childhood. Although it is very extensive and time consuming, its results are in great detail and reliable.
Nancy Andreasen preferred to identify TDs as thought-language-communication disorders (TLC disorders). Up to seven domains of FTD have been described on the Thought, Language, Communication (TLC) Scale, with most of the variance accounted for by two or three domains. Some TLC disorders are more suggestive of severe disorder, and are listed with the first 11 items.
Diagnoses
The DSM V categorizes FTD as "a psychotic symptom, manifested as bizarre speech and communication." FTD may include incoherence, peculiar words, disconnected ideas, or a lack of unprompted content expected from normal speech.Clinical psychologists typically assess FTD by initiating an exploratory conversation with patients and observing the patient's verbal responses.
FTD is often used to establish a diagnosis of schizophrenia; in cross-sectional studies, 27 to 80 percent of patients with schizophrenia present with FTD. A hallmark feature of schizophrenia, it is also widespread amongst other psychiatric disorders; up to 60 percent of those with schizoaffective disorder and 53 percent of those with clinical depression demonstrate FTD, suggesting that it is not exclusive to schizophrenia. About six percent of healthy subjects exhibit a mild form of FTD.
The characteristics of FTD vary amongst disorders. A number of studies indicate that FTD in mania is marked by irrelevant intrusions and pronounced combinatory thinking, usually with a playfulness and flippancy absent from patients with schizophrenia. The FTD present in patients with schizophrenia was characterized by disorganization, neologism, and fluid thinking, and confusion with word-finding difficulty.
There is limited data on the longitudinal course of FTD. The most comprehensive longitudinal study of FTD by 2023 found a distinction in the longitudinal course of thought-disorder symptoms between schizophrenia and other psychotic disorders. The study also found an association between pre-index assessments of social, work and educational functioning and the longitudinal course of FTD.
Possible causes
Several theories have been developed to explain the causes of formal thought disorder. It has been proposed that FTD relates to neurocognition via semantic memory.Semantic network impairment in people with schizophrenia—measured by the difference between fluency (e.g. the number of animals' names produced in 60 seconds) and phonological fluency (e.g. the number of words beginning with "F" produced in 60 seconds)—predicts the severity of formal thought disorder, suggesting that verbal information (through semantic priming) is unavailable. Other hypotheses include working memory deficit (being confused about what has already been said in a conversation) and attentional focus.
FTD in schizophrenia has been found to be associated with structural and functional abnormalities in the language network, where structural studies have found bilateral grey matter deficits; deficits in the bilateral inferior frontal gyrus, bilateral inferior parietal lobule and bilateral superior temporal gyrus are FTD correlates. Other studies did not find an association between FTD and structural aberrations of the language network, however, and regions not included in the language network have been associated with FTD. Future research is needed to clarify whether there is an association with FTD in schizophrenia and neural abnormalities in the language network.
Transmitter systems which might cause FTD have also been investigated. Studies have found that glutamate dysfunction, due to a rarefaction of glutamatergic synapses in the superior temporal gyrus in patients with schizophrenia, is a major cause of positive FTD.
The heritability of FTD has been demonstrated in a number of family and twin studies. Imaging genetics studies, using a semantic verbal-fluency task performed by the participants during functional MRI scanning, revealed that alleles linked to glutamatergic transmission contribute to functional aberrations in typical language-related brain areas. FTD is not solely genetically determined, however; environmental influences, such as allusive thinking in parents during childhood, and environmental risk factors for schizophrenia (including childhood abuse, migration, social isolation, and cannabis use) also contribute to the pathophysiology of FTD.
The origins of FTD have been theorised from a social-learning perspective. Singer and Wynne said that familial communication patterns play a key role in shaping the development of FTD; dysfunctional social interactions undermine a child's development of cohesive, stable mental representations of the world, increasing their risk of developing FTD.
Treatments
Antipsychotic medication is often used to treat FTD. Although the vast majority of studies of the efficacy of antipsychotic treatment do not report effects on syndromes or symptoms, six older studies report the effects of antipsychotic treatment on FTD. These studies and clinical experience indicate that antipsychotics are often an effective treatment for patients with positive or negative FTD, but not all patients respond to them.
Cognitive behavioural therapy (CBT) is another treatment for FTD, but its effectiveness has not been well-studied. Large randomised controlled trials evaluating the effectiveness of CBT for treating psychosis often exclude individuals with severe FTD because it reduces the therapeutic alliance required by the therapy. However, provisional evidence suggests that FTD may not preclude the effectiveness of CBT. Kircher and colleagues have suggested that the following methods should be used in CBT for patients with FTD:
- Practise structuring, summarising, and feedback methods
- Repeat and clarify the core issues and main emotions that the patient is trying to communicate
- Gently encourage patients to clarify what they are trying to communicate
- Ask patients to clearly state their communication goal
- Ask patients to slow down and explain how one point leads to another
- Help patients identify the links between ideas
- Identify the main affect linked to the thought disorder
- Normalise problems with thinking
Signs and symptoms
Language abnormalities exist in the general population, and do not necessarily indicate a condition. They can occur in schizophrenia and other disorders (such as mania or depression), or in anyone who may be tired or stressed. To distinguish thought disorder, patterns of speech, severity of symptoms, their frequency, and any resulting functional impairment can be considered.
Symptoms of TD include derailment,pressured speech, poverty of speech, tangentiality, and thought blocking. FTD is a hallmark feature of schizophrenia, but is also associated with other conditions (including mood disorders, dementia, mania, and neurological diseases). Impaired attention, poor memory, and difficulty formulating abstract concepts may also reflect TD, and can be observed and assessed with mental-status tests such as serial sevens or memory tests.
Types
Thirty symptoms (or features) of TD have been described, including:
- Alogia: A poverty of speech in amount or content, it is classified as a negative symptom of schizophrenia. When further classifying symptoms, poverty of speech content (little meaningful content with a normal amount of speech) is a disorganization symptom. Under SANS, thought blocking is considered a part of alogia, and so is increased latency in response.
- Thought blocking (also known as deprivation of thought and obstructive thought): An abrupt stop in the middle of a train of thought which may not be able to be continued.
- Circumstantial speech (also known as circumstantial thinking): An inability to answer a question without excessive, unnecessary detail. This differs from tangential thinking in that the person does eventually return to the original point. A patient may answer the question "How have you been sleeping lately?" with "Oh, I go to bed early, so I can get plenty of rest. I like to listen to music or read before bed. Right now I'm reading a good mystery. Maybe I'll write a mystery someday. But it isn't helping, reading I mean. I have been getting only 2 or 3 hours of sleep at night."
- Clanging: An instance where ideas are related only by similar or rhyming sounds rather than actual meaning. This may be heard as excessive rhyming or alliteration ("Many moldy mushrooms merge out of the mildewy mud on Mondays", or "I heard the bell. Well, hell, then I fell"). It is most commonly seen in the manic phase of bipolar disorder, although it is also often observed in patients with schizophrenia and schizoaffective disorder.
- Derailment (also known as loose association and knight's move thinking): Thought frequently moves from one idea to another which is obliquely related or unrelated, often appearing in speech but also in writing ("The next day when I'd be going out you know, I took control, like uh, I put bleach on my hair in California"),
- Distractible speech: In mid-speech, the subject is changed in response to a nearby stimulus ("Then I left San Francisco and moved to ... Where did you get that tie?")
- Echolalia: Echoing of another's speech, once or in repetition. It may involve repeating only the last few words (or the last word) of another person's sentences, and is common on the autism spectrum and in Tourette syndrome.
- Evasion: The next logical idea in a sequence is replaced with another idea closely (but not accurately or appropriately) related to it; also known as paralogia and perverted logic.
- Flight of ideas: A form of FTD marked by abrupt leaps from one topic to another, possibly with discernible links between successive ideas, perhaps governed by similarities between subjects or by rhyming, puns, wordplay, or innocuous environmental stimuli (such as the sound of birds chirping). It is most characteristic of the manic phase of bipolar disorder.
- Illogicality: Conclusions are reached which do not follow logically (non sequiturs or faulty inferences). "Do you think this will fit in the box?" is answered with, "Well of course; it's brown, isn't it?"
- Incoherence (word salad): Speech which is unintelligible because the individual words are real, but the manner in which they are strung together results in gibberish. The question "Why do people comb their hair?" elicits a response like "Because it makes a twirl in life, my box is broken help me blue elephant. Isn't lettuce brave? I like electrons, hello please!"
- Neologisms: Completely new words (or phrases) whose origins and meanings are usually unrecognizable ("I got so angry I picked up a dish and threw it at the geshinker"). They may also involve elisions of two words which are similar in meaning or sound. Although neologisms may refer to words formed incorrectly whose origins are understandable (such as "headshoe" for "hat"), these can be more clearly referred to as word approximations.
- Overinclusion: The failure to eliminate ineffective, inappropriate, irrelevant, extraneous details associated with a particular stimulus.
- Perseveration: Persistent repetition of words or ideas, even when another person tries to change the subject. ("It's great to be here in Nevada, Nevada, Nevada, Nevada, Nevada.") It may also involve repeatedly giving the same answer to different questions ("Is your name Mary?" "Yes." "Are you in the hospital?" "Yes." "Are you a table?" "Yes"). Perseveration can include palilalia and logoclonia, and may indicate an organic brain disease such as Parkinson's disease.
- Phonemic paraphasia: Mispronunciation; syllables out of sequence ("I slipped on the lice and broke my arm").
- Pressured speech: Rapid speech without pauses, which is difficult to interrupt.
- Referential thinking: Viewing innocuous stimuli as having a specific meaning for the self ("What's the time?" "It's 7 o'clock. That's my problem").
- Semantic paraphasia: Substitution of inappropriate words ("I slipped on the coat, on the ice I mean, and broke my book").
- Stilted speech: Speech characterized by words or phrases which are flowery, excessive, and pompous ("The attorney comported himself indecorously").
- Tangential speech: Wandering from the topic and never returning to it, or providing requested information ("Where are you from?" "My dog is from England. They have good fish and chips there. Fish breathe through gills").
- Verbigeration: Meaningless, stereotyped repetition of words or phrases which replace understandable speech; seen in schizophrenia.
Terminology
Psychiatric and psychological glossaries in 2015 and 2017 defined thought disorder' as disturbed thinking or cognition which affects communication, language, or thought content including poverty of ideas, neologisms, paralogia, word salad, and delusions (disturbances of thought content and form), and suggested the more-specific terms content thought disorder (CTD) and formal thought disorder (FTD). CTD was defined as a TD characterized by multiple fragmented delusions, and FTD was defined as a disturbance in the form or structure of thinking. The 2013 DSM-5 only used the term FTD, primarily as a synonym for disorganized thinking and speech. This contrasts with the 1992 ICD-10 (which only used the word "thought disorder", always accompanied with "delusion" and "hallucination") and a 2002 medical dictionary which generally defined thought disorders similarly to the psychiatric glossaries and used the word in other entries as the ICD-10 did.
A 2017 psychiatric text describing thought disorder as a "disorganization syndrome" in the context of schizophrenia:
"Thought disorder" here refers to disorganization of the form of thought and not content. An older use of the term "thought disorder" included the phenomena of delusions and sometimes hallucinations, but this is confusing and ignores the clear differences in the relationships between symptoms that have become apparent over the past 30 years. Delusions and hallucinations should be identified as psychotic symptoms, and thought disorder should be taken to mean formal thought disorders or a disorder of verbal cognition.
— Phenomenology of Schizophrenia (2017), THE SYMPTOMS OF SCHIZOPHRENIA
The text said that some clinicians use the term "formal thought disorder" broadly, referring to abnormalities in thought form with psychotic cognitive signs or symptoms, and studies of cognition and subsyndromes in schizophrenia may refer to FTD as conceptual disorganization or disorganization factor.
Some disagree:
Unfortunately, "thought disorder" is often involved rather loosely to refer to both FTD and delusional content. For the sake of clarity, the unqualified use of the phrase "thought disorder" should be discarded from psychiatric communication. Even the designation "formal thought disorder" covers too wide a territory. It should always be made clear whether one is referring to derailment or loose associations, flight of ideas, or circumstantiality.
— The Mental Status Examination, The Medical Basis of Psychiatry (2016)
Course, diagnosis, and prognosis
It was believed that TD occurred only in schizophrenia, but later findings indicate that it may occur in other psychiatric conditions (including mania) and in people without mental illness. Not all people with schizophrenia have a TD; the condition is not specific to the disease.
When defining thought-disorder subtypes and classifying them as positive or negative symptoms, Nancy Andreasen found that different subtypes of TD occur at different frequencies in those with mania, depression, and schizophrenia. People with mania have pressured speech as the most prominent symptom, and have rates of derailment, tangentiality, and incoherence as prominent as in those with schizophrenia. They are likelier to have pressured speech, distractibility, and circumstantiality.
People with schizophrenia have more negative TD, including poverty of speech and poverty of content of speech, but also have relatively high rates of some positive TD. Derailment, loss of goal, poverty of content of speech, tangentiality and illogicality are particularly characteristic of schizophrenia. People with depression have relatively-fewer TDs; the most prominent are poverty of speech, poverty of content of speech, and circumstantiality. Andreasen noted the diagnostic usefulness of dividing the symptoms into subtypes; negative TDs without full affective symptoms suggest schizophrenia.
She also cited the prognostic value of negative-positive-symptom divisions. In manic patients, most TDs resolve six months after evaluation; this suggests that TDs in mania, although as severe as in schizophrenia, tend to improve. In people with schizophrenia, however, negative TDs remain after six months and sometimes worsen; positive TDs somewhat improve. A negative TD is a good predictor of some outcomes; patients with prominent negative TDs are worse in social functioning six months later. More prominent negative symptoms generally suggest a worse outcome; however, some people may do well, respond to medication, and have normal brain function. Positive symptoms vary similarly.
A prominent TD at illness onset suggests a worse prognosis, including:
- illness begins earlier
- increased risk of hospitalization
- decreased functional outcomes
- increased disability rates
- increased inappropriate social behaviors
TD which is unresponsive to treatment predicts a worse illness course. In schizophrenia, TD severity tends to be more stable than hallucinations and delusions. Prominent TDs are more unlikely to diminish in middle age, compared with positive symptoms. Less-severe TD may occur during the prodromal and residual periods of schizophrenia. Treatment for thought disorder may include psychotherapy, such as cognitive behavior therapy (CBT), and psychotropic medications.
The DSM-5 includes delusions, hallucinations, disorganized thought process (formal thought disorder), and disorganized or abnormal motor behavior (including catatonia) as key symptoms of psychosis. Schizophrenia-spectrum disorders such as schizoaffective disorder and schizophreniform disorder typically consist of prominent hallucinations, delusions and FTD; the latter presents as severely disorganized, bizarre, and catatonic behavior. Psychotic disorders due to medical conditions and substance use typically consist of delusions and hallucinations. The rarer delusional disorder and shared psychotic disorder typically present with persistent delusions. FTDs are commonly found in schizophrenia and mood disorders, with poverty of speech content more common in schizophrenia.
Psychoses such as schizophrenia and bipolar mania are distinguishable from malingering, when an individual fakes illness for other gains, by clinical presentations; malingerers feign thought content with no irregularities in form such as derailment or looseness of association. Negative symptoms, including alogia, may be absent, and chronic thought disorder is typically distressing.
Autism spectrum disorders (ASD) whose diagnosis requires the onset of symptoms before three years of age can be distinguished from early-onset schizophrenia; schizophrenia under age 10 is extremely rare, and ASD patients do not display FTDs. However, it has been suggested that individuals with ASD display language disturbances like those found in schizophrenia; a 2008 study found that children and adolescents with ASD showed significantly more illogical thinking and loose associations than control subjects. The illogical thinking was related to cognitive functioning and executive control; the loose associations were related to communication symptoms and parent reports of stress and anxiety.
Rorschach tests have been useful for assessing TD in disturbed patients. A series of inkblots are shown, and patient responses are analyzed to determine disturbances of thought. The nature of the assessment offers insight into the cognitive processes of another, and how they respond to equivocal stimuli.Hermann Rorschach developed this test to diagnose schizophrenia after realizing that people with schizophrenia gave drastically different interpretations of Klecksographie inkblots from others whose thought processes were considered normal, and it has become one of the most widely-used assessment tools for diagnosing TDs.
The Thought Disorder Index (TDI), also known as the Delta Index, was developed to help further determine the severity of TD in verbal responses. TDI scores are primarily derived from verbally-expressed interpretations of the Rorschach test, but TDI can also be used with other verbal samples (including the Wechsler Adult Intelligence Scale). TDI has a twenty-three-category scoring index; each category scores the level of severity on a scale from 0–1, with .25 being mild and 1.00 being most severe (.25, .50, .75, 1.00).
Criticism
TD has been criticized as being based on circular or incoherent definitions. Symptoms of TD are inferred from disordered speech, based on the assumption that disordered speech arises from disordered thought. Although TD is typically associated with psychosis, similar phenomena can appear in different disorders and leading to misdiagnosis.
A criticism related to the separation of symptoms of schizophrenia into negative or positive symptoms, including TD, is that it oversimplifies the complexity of TD and its relationship to other positive symptoms.Factor analysis has found that negative symptoms tend to correlate with one another, but positive symptoms tend to separate into two groups. The three clusters became known as negative symptoms, psychotic symptoms, and disorganization symptoms. Alogia, a TD traditionally classified as a negative symptom, can be separated into two types: poverty of speech content as (a disorganization symptom) and poverty of speech, response latency, and thought blocking (negative symptoms). Positive-negative-symptom diametrics, however, may enable a more accurate characterization of schizophrenia.
See also
Further reading
- VandenBos GR, ed. (2015). APA dictionary of psychology (2nd ed.). Washington, DC: American Psychological Association. doi:10.1037/14646-000. ISBN 978-1-4338-1944-5.
- Sadock VA, Sadock BJ, Ruiz P, eds. (2017). Kaplan & Sadock's Comprehensive Textbook of Psychiatry (10th ed.). Wolters Kluwer. ISBN 978-1-4511-0047-1.
- Sadock BJ, Sadock VA (2008). Kaplan and Sadock's Concise Textbook of Clinical Psychiatry. Lippincott Williams & Wilkins. ISBN 9780781787468.
- Andreasen NC (2016). "25 Thought Disorder". In Fatemi SH, Clayton PJ (eds.). The Medical Basis of Psychiatry (4th ed.). New York: Springer Science+Business Media. pp. 497–505. doi:10.1007/978-1-4939-2528-5. ISBN 978-1-4939-2528-5.
- McKenna PJ, Oh TM (2005). Schizophrenic Speech: Making Sense of Bathroots and Ponds that Fall in Doorways. Cambridge University Press. ISBN 978-0-521-81075-3.
| Authority control: National |
|---|
