Eumycetoma
| Eumycetoma | |
|---|---|
| Other names | Madura foot |
 | |
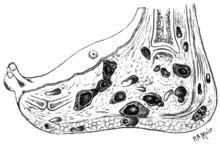
| An infected Foot | |
| Specialty | Infectious disease |
| Symptoms | Swelling, weeping pus filled sinuses, deformity. |
| Complications | amputation |
| Causes | Madurella spp., Leptosphaeria senegalensis, Curvularia lunata, Pseudallescheria spp., Neotestudina rosatii, Acremonium spp. and Fusarium spp. |
| Diagnostic method | Microscopy, biopsy, culture,medical imaging, ELISA, immunodiffusion, DNA sequencing |
| Differential diagnosis | Actinomycosis (Actinomycetoma) |
| Treatment | Surgical debridement, antifungal medicines |
| Medication | Itraconazole, posaconazole, voriconazole |
| Prognosis | Recurrence is common |
| Frequency | Endemic in Africa, India and South America |
Eumycetoma, also known as Madura foot, is a persistent fungal infection of the skin and the tissues just under the skin, affecting most commonly the feet, although it can occur in hands and other body parts. It starts as a painless wet nodule, which may be present for years before ulceration, swelling, grainy discharge and weeping from sinuses and fistulae, followed by bone deformity.
Several fungi can cause eumycetoma, including: Madurella mycetomatis, Madurella grisea, Leptosphaeria senegalensis, Curvularia lunata, Scedosporium apiospermum, Neotestudina rosatii, and Acremonium and Fusarium species. Diagnosis is by biopsy, visualising the fungi under the microscope and culture.Medical imaging may reveal extent of bone involvement. Other tests include ELISA, immunodiffusion, and DNA Barcoding.
Treatment includes surgical removal of affected tissue and antifungal medicines. After treatment, recurrence is common. Sometimes, amputation is required.
The infection occurs generally in the tropics, and is endemic in Sub-Saharan Africa, especially Sudan, India, parts of South America and Mexico. Few cases have been reported across North Africa. Mycetoma is probably low-endemic to Egypt with predilection for eumycetoma. In 2016, the World Health Organization recognised eumycetoma as a neglected tropical disease.
Signs and symptoms
The initial lesion is a small swelling under the skin following minor trauma. It appears as a painless wet nodule, which may be present for years before ulceration, swelling and weeping from sinuses, followed by bone deformity. The sinuses discharge a grainy liquid of fungal colonies. These grains are usually black or white. Destruction of deeper tissues, and deformity and loss of function in the affected limbs may occur in later stages. It tends to occur in one foot. Mycetoma due to bacteria has similar clinical features.
Causes
Eumycetoma is a type of mycetoma caused by fungi. Mycetoma caused by bacteria from the phylum Actinomycetes is different. Both have similar clinical features.
The most common fungi causing white discharge is Pseudallescheria boydii. Other causative agents of non-black grain eumycetoma include Acremonium and Fusarium species.
Black discharge tends to be caused by species from the genera Madurella, Pyrenochaeta, Exophiala, Leptosphaeria and Curvularia. The most common species are Madurella mycetomatis and Trematospheria grisea (previously called Madurella grisea).
Mechanism
The disease is acquired by entry of the fungal spores from the soil through a breach in the skin produced by minor trauma like a thorn prick. The disease then spreads to deeper tissues and also forms sinus tracts leading to skin surface. Mature lesions are characterised by a grainy discharge from these sinuses. These discharges contain fungal colonies and are infective. Spread of infection internally through blood or lymph is uncommon.
Infections that produce a black discharge mainly spread subcutaneously. In the red and yellow varieties deep spread occurs early, infiltrating muscles and bones but sparing nerves and tendons, which are highly resistant to the invasion.
Botryomycosis, also known as bacterial pseudomycosis, produces a similar clinical picture and is caused usually by Staphylococcus aureus. Other bacteria may also cause botryomycosis.
Diagnosis
Diagnosis is by biopsy, visualising the fungi under the microscope and culture, which show characteristic fungal filaments and vesicles characteristic of the fungi. Other tests include ELISA, immunodiffusion, and PCR with DNA sequencing (so-called DNA barcoding).
X rays and ultrasonography may be carried out to assess the extent of the disease. X rays findings are extremely variable. The disease is most often observed at an advanced stage that exhibits extensive destruction of all bones of the foot. Rarely, a single lesion may be seen in the tibia where the picture is identical with chronic osteomyelitis. Cytology of fine needle aspirate or pus from the lesion, and tissue biopsy may be undertaken sometimes. Some publications have claimed a "dot in a circle sign" as a characteristic MRI feature for this condition (this feature has also been described on ultrasound).
Differential diagnosis
The following clinical conditions may be considered before diagnosing a patient with mycetoma:
- Tuberculous ulcer
- Kaposi's sarcoma, a vascular tumour of skin usually seen in AIDS.
- Leprosy
- Syphilis
- Malignant neoplasm
- Tropical ulcer
- Botryomycosis, a skin infection usually caused by the bacteria Staphylococcus aureus.
Prevention
No vaccine is available. Simple hygienic precautions like wearing shoes or sandals while working in fields, and washing hands and feet at regular intervals may help prevent the disease.
Treatment
Surgery combined with itraconazole may be given for up to year when the grains are black.Posaconazole is another option.Voriconazole can be used for infections caused by Fusarium species.
Ketoconazole has been used to treat eumycetoma but has many side effects.Actinomycetes usually respond well to medical treatment, but eukaryotic infections are generally resistant and may require surgical interventions including salvage procedures as bone resection or even the more radical amputation.
Epidemiology
The disease is more common in males aged 20–40 years who work as labourers, farmers and herders, and in travellers to tropical regions, where the condition is endemic.
History
Madura foot or maduromycosis or maduramycosis is described in ancient writings of India as Padavalmika, which, translated means Foot anthill. The first modern description of Madura foot was made in 1842 from Madurai (the city after which the disease was named Madura-mycosis) in India, by Gill. The fungal cause of the disease was established in 1860 by Carter.
Society and culture
In 2016, the World Health Organization recognised eumycetoma as a neglected tropical disease. Traditionally occurring in regions where resources are scarce, medicines may be expensive and diagnosis is frequently made late, when more invasive treatment may be required.
External links
| Classification | |
|---|---|
| External resources |
|
Superficial and cutaneous (dermatomycosis): Tinea = skin; Piedra (exothrix/ endothrix) = hair |
|
||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Subcutaneous, systemic, and opportunistic |
|
||||||||||||||||||||||
| Mesomycetozoea | |||||||||||||||||||||||
| Ungrouped | |||||||||||||||||||||||