Tibolone
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Livial, Tibella, Tibofem, others |
| Other names | TIB; ORG-OD-14; 7α-Methylnoretynodrel; 7α-Methyl-17α-ethynyl-19-nor-δ5(10)-testosterone; 17α-Ethynyl-7α-methylestr-5(10)-en-17β-ol-3-one; 7α-Methyl-19-nor-17α-pregn-5(10)-en-20-yn-17-ol-3-one |
| AHFS/Drugs.com | Professional Drug Facts |
| Pregnancy category |
|
| Routes of administration |
By mouth |
| Drug class | Progestogen; Progestin; Estrogen; Androgen; Anabolic steroid |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 92% |
| Protein binding | 96.3% (to albumin; low affinity for SHBG) |
| Metabolism | Liver, intestines (hydroxyl-ation, isomerization, conjugation) |
| Metabolites | • Δ4-Tibolone • 3α-Hydroxytibolone • 3β-Hydroxytibolone • Sulfate conjugates |
| Elimination half-life | 45 hours |
| Excretion |
Urine: 40% Feces: 60% |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank |
|
| ChemSpider |
|
| UNII | |
| KEGG |
|
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.024.609 |
| Chemical and physical data | |
| Formula | C21H28O2 |
| Molar mass | 312.453 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Tibolone, sold under the brand name Livial among others, is a medication which is used in menopausal hormone therapy and in the treatment of postmenopausal osteoporosis and endometriosis. The medication is available alone and is not formulated or used in combination with other medications. It is taken by mouth.
Side effects of tibolone include acne and increased hair growth among others. Tibolone is a synthetic steroid with weak estrogenic, progestogenic, and androgenic activity, and hence is an agonist of the estrogen, progesterone, and androgen receptors. It is a prodrug of several metabolites. The estrogenic effects of tibolone may show tissue selectivity in their distribution.
Tibolone was developed in the 1960s and was introduced for medical use in 1988. It is marketed widely throughout the world. The medication is not available in the United States.
Medical uses
Tibolone is used in the treatment of menopausal symptoms like hot flashes and vaginal atrophy, postmenopausal osteoporosis, and endometriosis. It has similar or greater effectiveness compared to older menopausal hormone therapy medications, but shares a similar side effect profile. It has also been investigated as a possible treatment for female sexual dysfunction.
Tibolone reduces hot flashes, prevents bone loss, improves vaginal atrophy and urogenital symptoms (e.g., vaginal dryness, dyspareunia), and has positive effects on mood and sexual function. The medication may have greater benefits on libido than standard menopausal hormone therapy, which may be related to its androgenic effects. It is associated with low rates of vaginal bleeding and breast pain.
A 2015 network meta-analysis of randomized controlled trials found that tibolone was associated with a significantly decreased risk of breast cancer (RR = 0.317). The decrease in risk was greater than that observed with most of the aromatase inhibitors and selective estrogen receptor modulators that were included in the analysis. However, paradoxically, other research has found evidence supporting an increased risk of breast cancer with tibolone.
Available forms
Tibolone is available in the form of 2.5 mg oral tablets. It is typically used once daily at a dosage of 1.25 or 2.5 mg.
Side effects
A report in September 2009 from Health and Human Services' Agency for Healthcare Research and Quality suggests that tamoxifen, raloxifene, and tibolone used to reduce the risk of breast cancer significantly reduce the occurrence of invasive breast cancer in midlife and older women, but also increase the risk of adverse effects.
Tibolone can infrequently produce androgenic side effects such as acne and increased facial hair growth. Such side effects have been found to occur in 3 to 6% of treated women.
A 2016 Cochrane review has been published on the short-term and long-term effects of tibolone, including adverse effects. Possible adverse effects of tibolone include unscheduled vaginal bleeding (OR = 2.79; incidence 13–26% more than placebo), an increased risk of breast cancer in women with a history of breast cancer (OR = 1.5) although apparently not without a history of breast cancer (OR = 0.52), an increased risk of cerebrovascular events (strokes) (OR = 1.74) and cardiovascular events (OR = 1.38), and an increased risk of endometrial cancer (OR = 2.04). However, most of these figures are based on very low-quality evidence.
Tibolone has been associated with increased risk of endometrial cancer in most studies.
Pharmacology
Pharmacodynamics
Tibolone possesses a complex pharmacology and has weak estrogenic, progestogenic, and androgenic activity. Tibolone, 3α-hydroxytibolone, and 3β-hydroxytibolone act as agonists of the estrogen receptors. Tibolone and its metabolite δ4-tibolone act as agonists of the progesterone and androgen receptors, while 3α-hydroxytibolone and 3β-hydroxytibolone, conversely, act as antagonists of these receptors. Relative to other progestins, tibolone, including its metabolites, has been described as possessing moderate functional antiestrogenic activity (that is, progestogenic activity), moderate estrogenic activity, high androgenic activity, and no clinically significant glucocorticoid, antiglucocorticoid, mineralocorticoid, or antimineralocorticoid activity. The ovulation-inhibiting dosage of tibolone is 2.5 mg/day.
Estrogenic activity
Tibolone and its two major active metabolites, 3α-hydroxytibolone and 3β-hydroxytibolone, act as potent, fully activating agonists of the estrogen receptor (ER), with a high preference for the ERα. These estrogenic metabolites of tibolone have much weaker activity as estrogens than estradiol (e.g., have 3–29% of the affinity of estradiol for the ER), but occur at relatively high concentrations that are sufficient for full and marked estrogenic responses to occur.
The estrogenic effects of tibolone show tissue selectivity in their distribution, with desirable effects in bone, the brain, and the vagina, and lack of undesirable action in the uterus, breast, and liver. The observations of tissue selectivity with tibolone have been theorized to be the result of metabolism, enzyme modulation (e.g., of estrogen sulfatase and estrogen sulfotransferase), and receptor modulation that vary in different target tissues. This selectivity differs mechanistically from that of selective estrogen receptor modulators (SERMs) such as tamoxifen, which produce their tissue selectivity via means of modulation of the ER. As such, to distinguish it from SERMs, tibolone has been variously described as a "selective tissue estrogenic activity regulator" (STEAR), "selective estrogen enzyme modulator" (SEEM), or "tissue-specific receptor and intracrine mediator" (TRIM). More encompassingly, tibolone has also been described as a "selective progestogen, estrogen, and androgen regulator" (SPEAR), which is meant to reflect the fact that it is tissue-selective and that it regulates effects not only of estrogens but of all three of the major sex hormone classes. Although indications of tissue selectivity with tibolone have been observed, the medication has paradoxically nonetheless been associated with increased risk of endometrial cancer and breast cancer in clinical studies.
It was reported in 2002 that tibolone or its metabolite δ4-tibolone is transformed by aromatase into the potent estrogen 7α-methylethinylestradiol in women, analogously to the transformation of norethisterone into ethinylestradiol. Controversy and disagreement followed when other researchers contested the findings however. By 2008, these researchers had asserted that tibolone is not aromatized in women and that the previous findings of 7α-methylethinylestradiol detection were merely a methodological artifact. In accordance, a 2009 study found that an aromatase inhibitor had no effect on the estrogenic potencies of tibolone or its metabolites in vitro, unlike the case of testosterone. In addition, another 2009 study found that the estrogenic effects of tibolone on adiposity in rats do not require aromatization (as indicated by the use of aromatase knockout mice), further in support that 3α-hydroxytibolone and 3β-hydroxytibolone are indeed responsible for such effects. These findings are also in accordance with the fact that tibolone decreases sex hormone-binding globulin (SHBG) levels by 50% in women and does not increase the risk of venous thromboembolism (VTE) (RR = 0.92), which would not be expected if the medication formed a potent, liver metabolism-resistant estrogen similar to ethinylestradiol in important quantities. (For comparison, combined oral contraceptives containing ethinylestradiol, due mostly or completely to the estrogen component, have been found to increase SHBG levels by 200 to 400% and to increase the risk of VTE by about 4-fold (OR = 4.03).)
In spite of the preceding, others have held, as recently as 2011, that tibolone is converted into 7α-methylethinylestradiol in small quantities. They have claimed that 19-nortestosterone derivatives like tibolone, due to lacking a C19 methyl group, indeed are not substrates of the classical aromatase enzyme, but instead are still transformed into the corresponding estrogens by other cytochrome P450 monooxygenases. In accordance, the closely structurally related AAS trestolone (7α-methyl-19-nortestosterone or 17α-desethynyl-δ4-tibolone) has been found to be transformed into 7α-methylestradiol by human placental microsomes in vitro. Also in accordance, considerably disproportionate formation of ethinylestradiol occurs when norethisterone is taken orally (and hence undergoes first-pass metabolism in the liver) relative to parenterally, despite the absence of aromatase in the adult human liver.
Progestogenic activity
Tibolone and δ4-tibolone act as agonists of the progesterone receptor (PR). Tibolone has low affinity of 6% of that of promegestone for the PR, while δ4-tibolone has high affinity of 90% of that of promegestone for the PR. In spite of its high affinity for the PR however, δ4-tibolone possesses only weak progestogenic activity, about 13% of that of norethisterone. The weak progestogenic activity of tibolone may not be sufficient to fully counteract estrogenic activity of tibolone in the uterus and may be responsible for the increased risk of endometrial cancer that has been observed with tibolone in women in large cohort studies.
Androgenic activity
Tibolone, mainly via δ4-tibolone, has androgenic activity. Whereas tibolone itself has only about 6% of the affinity of metribolone for the androgen receptor, δ4-tibolone has relatively high affinity of about 35% of the affinity of metribolone for this receptor. At typical clinical dosages in women, the androgenic effects of tibolone are weak. However, relative to other 19-nortestosterone progestins, the androgenic activity of tibolone is high, with a potency comparable to that of testosterone. Indeed, the androgenic effects of tibolone have been ranked as stronger than those of all other commonly used 19-nortestosterone progestins (e.g., norethisterone, levonorgestrel, others).
The androgenic effects of tibolone have been postulated to be involved in the reduced breast cell proliferation, reduced breast cancer risk, improvement in sexual function, less unfavorable changes in hemostatic parameters relative to estrogen–progestogen combinations, and changes in liver protein synthesis (e.g., 30% reductions in HDL cholesterol levels, 20% reduction in triglyceride levels, and 50% reduction in SHBG levels) observed with tibolone. They are also responsible for the androgenic side effects of tibolone such as acne and increased hair growth in some women.
Other activities
Tibolone, 3α-hydroxytibolone, and 3β-hydroxytibolone act as antagonists of the glucocorticoid and mineralocorticoid receptors, with preference for the mineralocorticoid receptor. However, their affinities for these receptors are low, and tibolone has been described as possessing no clinically significant glucocorticoid, antiglucocorticoid, mineralocorticoid, or antimineralocorticoid activity.
Pharmacokinetics
The mean oral bioavailability of tibolone is 92%. Its plasma protein binding is 96.3%. It is bound to albumin, and both tibolone and its metabolites have low affinity for SHBG. Tibolone is metabolized in the liver and intestines. It is a prodrug and is rapidly transformed into several metabolites, including δ4-tibolone, 3α-hydroxytibolone, and 3β-hydroxytibolone, as well as sulfate conjugates of these metabolites. 3α-Hydroxytibolone is formed by 3α-hydroxysteroid dehydrogenase, 3β-hydroxytibolone is formed by 3β-hydroxysteroid dehydrogenase, δ4-tibolone is formed by Δ5-4-isomerase, and the sulfate conjugates of tibolone and its metabolites are formed by sulfotransferases, mainly SULT2A1. The sulfate conjugates can be transformed back into free steroids by steroid sulfatase. Following a single oral dose of 2.5 mg tibolone, peak serum levels of tibolone were 1.6 ng/mL, of δ4-tibolone were 0.8 ng/mL, of 3α-hydroxytibolone were 16.7 ng/mL, and of 3β-hydroxytibolone were 3.7 ng/mL after 1 to 2 hours. The elimination half-life of tibolone is 45 hours. It is excreted in urine 40% and feces 60%.
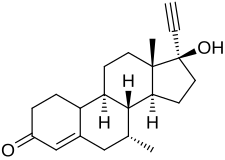
Chemistry
Tibolone, also known as 7α-methylnoretynodrel, as well as 7α-methyl-17α-ethynyl-19-nor-δ5(10)-testosterone or as 7α-methyl-17α-ethynylestr-5(10)-en-17β-ol-3-one, is a synthetic estrane steroid and a derivative of testosterone and 19-nortestosterone. It is more specifically a derivative of norethisterone (17α-ethynyl-19-nortestosterone) and is a member of the estrane subgroup of the 19-nortestosterone family of progestins. Tibolone is the 7α-methyl derivative of the progestin noretynodrel (17α-ethynyl-δ5(10)-19-nortestosterone). Other steroids related to tibolone include the progestin norgesterone (17α-vinyl-δ5(10)-19-nortestosterone) and the anabolic steroids trestolone (7α-methyl-19-nortestosterone) and mibolerone (7α,17α-dimethyl-19-nortestosterone).
History
Tibolone was developed in the 1960s. It was first introduced in the Netherlands in 1988, and was subsequently introduced in the United Kingdom in 1991.
Society and culture
Generic names
Tibolone is the generic name of the drug and its INN, USAN, BAN, DCF, and JAN. It is also known by its developmental code name ORG-OD-14.
Brand names
Tibolone is marketed under the brand names Livial, Tibofem, and Ladybon among others.
Availability
Tibolone is used widely in the European Union, Asia, Australasia, and elsewhere in the world, but is not available in the United States.
Legal status
Tibolone is a Schedule IV controlled substance in Canada under the 1996 Controlled Drugs and Substances Act. It is classified as an anabolic steroid under this act, due to its relatively high activity as an AR agonist, and is the only norethisterone (17α-ethynyl-19-nortestosterone) derivative that is classified as such. Tibolone is banned by WADA as an anabolic steroid category S1 largely due to its conversion to the delta-4 tibolone metabolite, which is a potent androgen.
Further reading
- "Tibolone (Livial)--a new steroid for the menopause". Drug and Therapeutics Bulletin. 29 (20): 77–78. September 1991. PMID 1935591.
- Ross LA, Alder EM (February 1995). "Tibolone and climacteric symptoms". Maturitas. 21 (2): 127–136. doi:10.1016/0378-5122(94)00888-E. PMID 7752950.
- Rymer JM (June 1998). "The effects of tibolone". Gynecological Endocrinology. 12 (3): 213–220. doi:10.3109/09513599809015548. PMID 9675570.
- Ginsburg J, Prelevic GM (1999). "Tibolone and the serum lipid/lipoprotein profile: does this have a role in cardiovascular protection in postmenopausal women?". Menopause. 6 (2): 87–89. doi:10.1097/00042192-199906020-00002. PMID 10374212.
- Gompel A, Jacob D, de Chambine S, Mimoun M, Decroix Y, Rostene W, Poitout P (May 1999). "[Action of SERM and SAS (tibolone) on breast tissue]". Contraception, Fertilité, Sexualité (in French). 27 (5): 368–375. PMID 10401183.
- Maudelonde T, Brouillet JP, Pujol P (September 1999). "[Anti-estrogens, selective estrogen receptor modulators (SERM), tibolone: modes of action]". Contraception, Fertilite, Sexualite (in French). 27 (9): 620–624. PMID 10540506.
- von Holst T (April 2000). "[Alternatives to hormone replacement therapy: raloxifene and tibolone]". Zeitschrift Fur Arztliche Fortbildung und Qualitatssicherung (in German). 94 (3): 205–209. PMID 10802895.
- Palacios S (January 2001). "Tibolone: what does tissue specific activity mean?". Maturitas. 37 (3): 159–165. doi:10.1016/S0378-5122(00)00184-5. PMID 11173177.
- Kloosterboer HJ (2001). "Tibolone: a steroid with a tissue-specific mode of action". The Journal of Steroid Biochemistry and Molecular Biology. 76 (1–5): 231–238. doi:10.1016/S0960-0760(01)00044-9. PMID 11384882. S2CID 8139376.
- "Tibolone: new type of hormone replacement". Harvard Women's Health Watch. 9 (5): 5. December 2001. PMID 11751099.
- Modelska K, Cummings S (January 2002). "Tibolone for postmenopausal women: systematic review of randomized trials". The Journal of Clinical Endocrinology and Metabolism. 87 (1): 16–23. doi:10.1210/jcem.87.1.8141. PMID 11788614.
- Gorai I (March 2002). "[Drugs in development for the treatment of osteoporosis: Tibolone]". Nihon Rinsho. Japanese Journal of Clinical Medicine (in Japanese). 60 (Suppl 3): 552–571. PMID 11979954.
- Jamin C, Poncelet C, Madelenat P (September 2002). "[Tibolone]". Presse Médicale (in French). 31 (28): 1314–1322. PMID 12355994.
- Reginster JY (October 2002). "[Postmenopausal hormonal treatment: conventional hormone replacement therapy or tibolone? Effects on bone]". Journal de Gynécologie, Obstétrique et Biologie de la Reproduction (in French). 31 (6): 541–549. PMID 12407324.
- Kloosterboer HJ, Ederveen AG (December 2002). "Pros and cons of existing treatment modalities in osteoporosis: a comparison between tibolone, SERMs and estrogen (+/-progestogen) treatments". The Journal of Steroid Biochemistry and Molecular Biology. 83 (1–5): 157–165. doi:10.1016/S0960-0760(03)00055-4. PMID 12650712. S2CID 25443489.
- de Gooyer ME, Deckers GH, Schoonen WG, Verheul HA, Kloosterboer HJ (January 2003). "Receptor profiling and endocrine interactions of tibolone". Steroids. 68 (1): 21–30. doi:10.1016/S0039-128X(02)00112-5. PMID 12475720. S2CID 40426061.
- Swegle JM, Kelly MW (May 2004). "Tibolone: a unique version of hormone replacement therapy". The Annals of Pharmacotherapy. 38 (5): 874–881. doi:10.1345/aph.1D462. PMID 15026563. S2CID 20473128.
- Gorai I (February 2004). "[Tibolone]". Nihon Rinsho. Japanese Journal of Clinical Medicine (in Japanese). 62 (Suppl 2): 555–559. PMID 15035189.
- Devogelaer JP (April 2004). "A review of the effects of tibolone on the skeleton". Expert Opinion on Pharmacotherapy. 5 (4): 941–949. doi:10.1517/14656566.5.4.941. PMID 15102576. S2CID 25827970.
- Reed MJ, Kloosterboer HJ (August 2004). "Tibolone: a selective tissue estrogenic activity regulator (STEAR)". Maturitas. 48 (Suppl 1): S4–S6. doi:10.1016/j.maturitas.2004.02.013. PMID 15337241.
- Kloosterboer HJ (August 2004). "Tissue-selectivity: the mechanism of action of tibolone". Maturitas. 48 (Suppl 1): S30–S40. doi:10.1016/j.maturitas.2004.02.012. PMID 15337246.
- Kloosterboer HJ (September 2004). "Tissue-selective effects of tibolone on the breast". Maturitas. 49 (1): S5–S15. doi:10.1016/j.maturitas.2004.06.022. PMID 15351102.
- von Schoultz B (September 2004). "The effects of tibolone and oestrogen-based HT on breast cell proliferation and mammographic density". Maturitas. 49 (1): S16–S21. doi:10.1016/j.maturitas.2004.06.011. PMID 15351103.
- Liu JH (December 2005). "Therapeutic effects of progestins, androgens, and tibolone for menopausal symptoms". The American Journal of Medicine. 118 (12): 88–92. doi:10.1016/j.amjmed.2005.09.040. PMID 16414332.
- Verheul HA, Kloosterboer HJ (December 2006). "Metabolism of exogenous sex steroids and effect on brain functions with a focus on tibolone". The Journal of Steroid Biochemistry and Molecular Biology. 102 (1–5): 195–204. doi:10.1016/j.jsbmb.2006.09.037. PMID 17113982. S2CID 33499701.
- Ettinger B (May 2007). "Tibolone for prevention and treatment of postmenopausal osteoporosis". Maturitas. 57 (1): 35–38. doi:10.1016/j.maturitas.2007.02.008. PMID 17350774.
- Notelovitz M (January 2007). "Postmenopausal tibolone therapy: biologic principles and applied clinical practice". MedGenMed. 9 (1): 2. PMC 1924982. PMID 17435612.
- Jacobsen DE, Samson MM, Kezic S, Verhaar HJ (September 2007). "Postmenopausal HRT and tibolone in relation to muscle strength and body composition". Maturitas. 58 (1): 7–18. doi:10.1016/j.maturitas.2007.04.012. PMID 17576043.
- Campisi R, Marengo FD (2007). "Cardiovascular effects of tibolone: a selective tissue estrogenic activity regulator". Cardiovascular Drug Reviews. 25 (2): 132–145. doi:10.1111/j.1527-3466.2007.00007.x. PMID 17614936.
- Carranza Lira S (October 2008). "[Relation between hormonal therapy and tibolone with SERMs in postmenopausal women's myomes growth]". Ginecologia y Obstetricia de Mexico (in Spanish). 76 (10): 610–614. PMID 19062511.
- Huang KE, Baber R (August 2010). "Updated clinical recommendations for the use of tibolone in Asian women". Climacteric. 13 (4): 317–327. doi:10.3109/13697131003681458. PMC 2942871. PMID 20443720.
- Biglia N, Maffei S, Lello S, Nappi RE (November 2010). "Tibolone in postmenopausal women: a review based on recent randomised controlled clinical trials". Gynecological Endocrinology. 26 (11): 804–814. doi:10.3109/09513590.2010.495437. PMID 20586550. S2CID 7203038.
- Kotani K, Sahebkar A, Serban C, Andrica F, Toth PP, Jones SR, et al. (September 2015). "Tibolone decreases Lipoprotein(a) levels in postmenopausal women: A systematic review and meta-analysis of 12 studies with 1009 patients". Atherosclerosis. 242 (1): 87–96. doi:10.1016/j.atherosclerosis.2015.06.056. PMID 26186655.
- Pinto-Almazán R, Segura-Uribe JJ, Farfán-García ED, Guerra-Araiza C (2017). "Effects of Tibolone on the Central Nervous System: Clinical and Experimental Approaches". BioMed Research International. 2017: 8630764. doi:10.1155/2017/8630764. PMC 5278195. PMID 28191467.
- Anagnostis P, Galanis P, Chatzistergiou V, Stevenson JC, Godsland IF, Lambrinoudaki I, et al. (May 2017). "The effect of hormone replacement therapy and tibolone on lipoprotein (a) concentrations in postmenopausal women: A systematic review and meta-analysis". Maturitas. 99: 27–36. doi:10.1016/j.maturitas.2017.02.009. hdl:10044/1/48763. PMID 28364865.
- Løkkegaard EC, Mørch LS (June 2018). "Tibolone and risk of gynecological hormone sensitive cancer". International Journal of Cancer. 142 (12): 2435–2440. doi:10.1002/ijc.31267. PMID 29349823.
External links
- "Tibolone". Drug Information Portal. U.S. National Library of Medicine.
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Corporate directors | |||
|---|---|---|---|
| Subsidiaries | |||
| Products |
|
||
| Facilities | |||
| Publications | |||